After two brain injuries, the most recent from a motor vehicle collision in 2015, 67-year-old Margaret despaired, saying,“I can’t keep living like this.” She was severely depressed and extremely anxious. She could barely leave her house and second-guessed even the most banal of social interactions. She was taking a high dose of Lexapro, lithium orotate, and various antiinflammatory supplements, and seeing a talented therapist, but she could not shake her awful mood. She was often irritable and afraid,and feared she was alienating those closest to her. She had been seeing a functional neurologist and had great success functionally but her mood was another story. So she decided to try transcranial magnetic stimulation, or TMS.
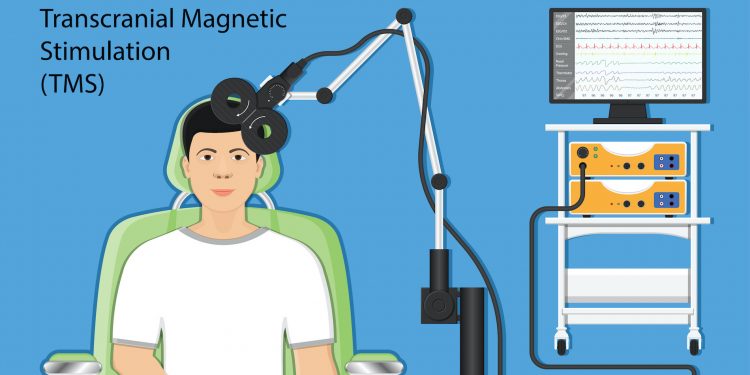
TMS utilizes an MRI-strength magnet, a 1.5 Tesla (electromagnetic) coil, that is placed directly on the skull and transmits an electromagnetic signal through the scalp, skull, and about 2.5 to 3.5cm deep into the cortex and connects to other brain structures that we know are implicated in depression, anxiety, trauma, and brain injury.
Prior to using a magnet to induce electricity, a direct electrical current was used, but it caused discomfort. TMS is much more precise. The TMS magnet fires into an area called the left dorsolateral prefrontal cortex (DL PFC) an area rich in terms of its connectome.
TMS is not a new technology. First invented in the mid-1980s, the FDA approved it for treatment-resistant major depressive disorder in 2008, and more recently for obsessive compulsive disorder. As part of our integrative practice with Northwest Functional Neurology, we offer rTMS for our patients who experience various neurological problems, including recovery from brain injuries.
The brain is a complex series of networks. Three that are very important in anxiety, depression, trauma and TBIs are the default mode network, (DMN), the salience network, and the executive network. The default mode network is what some people describe as being as close to a neuroanatomic description of “the seat of consciousness” as we have. It is the neurological basis for the self. It is our autobiographical information and includes memories of collection of events, facts about one’s self, and self-reference. As I often say, when you wake up in the morning and you look at your ceiling fan, you don’t have to think about who you are, you already know. You know coffee or tea. You know that annoying boy you went to fourth grade with. You know that person you had a crush on in college. You don’t have to “onboard” that information each day . It’s there with you at rest, which is why, some alternately refer to the DMN as the “resting state network.”
The DMN is most active when the brain is at rest or involved in social communication. In “healthy” people, its activity is attenuated during the performance of cognitively demanding tasks. That is, our salience network (salience meaning “important noticing”) can take us from a delightful mind wander to our “business brain,” where we are solving problems, paying attention, and making decisions. What happens in anxiety, depression, trauma, and brain injury, though, is that SN cannot handily move us from our restful brain to our working brain and it over-accentuates painful aspects of ourselves such as negative characteristics or painful memories. It keeps patients stuck in a loop of misery because it cannot easily switch over to the problem-solving part of our brain. TMS directly targets the executive network and the salience network to help get those brain structures working properly!
Although we do specialized treatment at Framework Functional Psychiatry and TMS (Northwest Functional Neurology), most of our patients benefit from “treatment as usual” and using the left DLPFC as our treatment target. Medical research has shown that the DMN is typically disrupted in TBIs.
Margaret completed the standard 36 TMS treatments and began to achieve results — both in terms of mood and congnition — as early as week two. She first feared that it wasn’t real. “Maybe it’s just a placebo,” she said. She continued to improve and finally wrote this in her correspondence for Christmas 2019: “Well, it’s been a long hard haul I say as I look back on these two head injuries phase of my life since 2015, but this afternoon I note a rather large yet subtle change in myself that is — miracle of miracles — seeping through the darkness, the parts of me that had disappeared, that I had forgotten ever existed, like my memory, my personality, my vitality, joy, words, perception, energy, and on and on. I knew I wasn’t myself and I had no capacity to access what I couldn’t even remember. I’m so happy to see my old familiar self make an appearance. She reminds me of all the people I love and have felt connected to throughout my life!”
Shauna Hahn specializes in the treatment of post-brain injury psychiatric disorders and often lectures on this topic. Shauna is excited to bring her expertise to TMS at her beautiful destination clinic, Framework Functional Psychiatry and TMS, in Lake Oswego, Oregon. www.frameworktms.com