By Kelly Harrigan
Treatments for concussions and head injuries are reaching new heights of awareness in recent years. Traditional medical standard of care has been a “wait and see” approach, which isn’t helpful for those who are afflicted. Traumatic brain injury (TBI) and post-concussive syndrome (PCS) often includes the many systems within the body, including musculoskeletal, nervous, circulatory, digestive, and visceral, with wide-ranging symptoms involving headaches and neck pain, which can cause tinnitus, vision problems, fatigue, anxiety, depression, irritability, cognitive issues pertaining to memory and concentration, as well as personality changes, all of which require a focus on a full-body approach to treatment.
Interest and investigation of manual therapies addressing the neurological tissues of the brain has increased in recent years as treatment for persons with TBI and PCS are currently stepping into the spotlight.
Why is this important?
It’s important because the brain continually seeks feedback from the body in order to maintain homeostasis. There are more than twice the number of sensory nerves than motor nerves within your body and your body relies on your senses more than movement to self-correct. Many sensors are located in the derma and subcutaneous layer (think skin), ligaments, joints, muscles, and also the fascia surrounding muscle fiber. The sensory nerves within the fascia contribute to delayed onset of muscle soreness.
At the same time, TBI and PCS can affect glial cells within the nervous system. The glial matrix forms the supportive structure of the brain, which is similar to fascial tissue. Manual therapies are thought to not only improve connectivity and communication of the glial network but that of the fascial network as well.
Can I get a connection?
The body’s systems are enveloped in fascia: interactive, interdependent, and interconnective tissues forming a complex network used in force transmissions, sensory functions, and wound regulation, yet also enabling optimal functioning and resiliency, allowing the body to repair stress, illness, injury, and physical and emotional trauma. You could say everything in your body that isn’t a cell is a fascia, with fascia providing the structure for your cells.
Our bodies respond to disruptions by creating tension points deep within the fascial network that our bodies are then forced to maneuver around. These shortcuts become imbalances within the fascial system and are seen in fascial shortening, dehydration, or thickening, thus impairing muscle function and mobility throughout the body.
We experience these functional and structural issues as pain, decreased flexibility, impaired movement, or various diseases. In fact, increased proprioceptive communications and connectivity is often stunted after a TBI.
I took the road less traveled…
But my body took the left turn at Albuquerque. (Only in COVID times, could you find a Robert Frost reference on the same road as Bugs Bunny…) Whatever and wherever the tension point, the body will take the path of least resistance. If you are experiencing stiffness, pain, or decreased mobility, the body will shift within itself, resulting in an altered axis of movement. In other words, your body is picking up bad habits, which explains why a person’s pain may be far removed from the initial site of symptoms.
Manual therapies assist and boost the body’s healing forces by easing tensions and restrictions along your fascial system, allowing your body to readily adapt to its environment. By treating one area you facilitate change and improvement in other areas. Like what improvements? Well, decreased depression, head pain, brain fog, and cervicogenic pain, increased cervical motion, improved sleep and quality of life, and even better mental clarity of focus. These manual therapeutics are non-invasive with positive results and almost no side effects.
Manual therapy is beneficial years after the original injury and maximizes the potential for full recovery when used in conjunction with other treatments. People may see benefits in only a few sessions, although lasting efficacy may need more frequent sessions.
The intriguing part of all of this is how mindfulness relates to movement and why we need to train our muscles to connect with our mind to remember the proper movements for optimal recovery. I was lucky enough to grab a quick interview and a short session with Kristin Erin, CEO of Mainsail Wellness and Performance (with our dogs, Winston, George, and Ella). Mainsail offers a multidisciplinary approach to TBI/PCS clients. The following is a snapshot of our chat.
What led you to mindful movement?
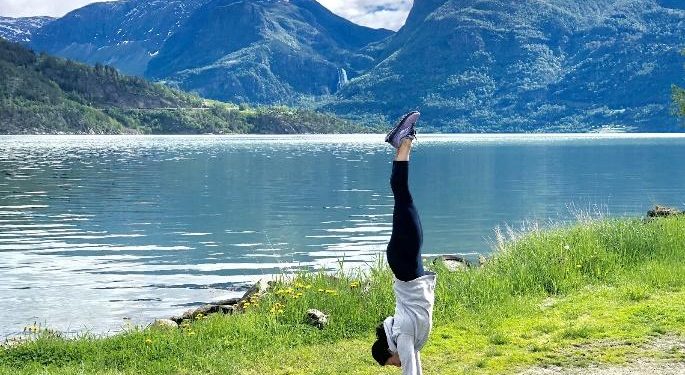
Growing up, movement was always incorporated in my everyday life. It brought me joy, confidence, and where I felt most like myself. In a sense, movement was my home. My love for movement, combined with my desire for challenge, ultimately led me to a lifetime of elite athletics. My parents were smart, directing my energy to gymnastics where I spent six years competing with USA Gymnastics, and later spent three years competing with USA Diving. Being involved with these sports while being trained by some of the best coaches in the world taught me the power mental focus has on physical performance.
Just as I was reaching new levels athletically, life threw a curve ball (as many of our readers can relate to). During my freshman year of college, I was diagnosed with a debilitating case of Lyme disease that went misdiagnosed for years. Days that were once filled with training were now filled with rest. My experience with Lyme disease was truly life-changing. For seven years I felt like a stranger in my body. I lived in a state where I was depleted of energy, lacked mental focus and the ability to sleep for any length of time because of pain. I knew that was not the life I wanted to live.
In order to make progress, I knew I had to apply the same dedication and mental focus I used in athletics to recovery. Each day I took one small step forward, followed by another small step. Over seven years those small steps were made up of visualization, breathing, and micromovements to re-establish a mind-body connection. Even though progress was slow, eventually I started feeling like myself again.
My road back to optimal health introduced me to the world of integrative approaches in medicine. Specifically, mind-body interventions through Pilates, yoga, fascial movement, and meditation. I quickly learned that traditional allopathic approaches could only take me so far, and I needed to incorporate outside support to bridge the gap back to full health. Once well enough, I decided to take another small step in participating in STOTT Pilates teacher-training education. That small step launched me into a career as an international mind-body educator.
Most recently, I founded Mainsail Wellness and Performance, which evolved from my experiences and the desire to provide others with an integrative mind-body approach to well-being through mindful movement and coaching.
Would you describe what you mean by mindful movement?
Mindful movement, when broken down into its most simplistic form, is the combination of mindfulness plus movement. Mindfulness means to be aware, and movement, in this sense, refers to physical training. Mindfulness is a method utilized to train our attention, and therefore is a tool to help train our brain. In recent years, research has grown exponentially in the field of neuroscience. the growth has expanded our understanding of brain physiology and brain behavior in response to mindfulness. Promising research dedicated to supporting people living with TBI report improvements in mental clarity, concentration, mood, and overall health. Mindfulness acts as a powerful driver to help shape our brain, and when combined directly with movement allows individuals to gain a greater sense of their own needs while rebuilding physical strength.
At Mainsail, we support clients in cultivating mindfulness directly through movement. Every movement completed is done with proprioceptive awareness and direct feedback. We acknowledge the critical role the brain plays in orchestrating physical functioning, as well as the fluctuation that occurs on the road to recovery. In order to best meet the needs of our clients, we build individually tailored movement programs guided by modern principles of rehabilitation. It is our goal to have a place where individuals can practice safely, effectively, and guild a greater sense of confidence in their own ability.
Why is this beneficial to people dealing with PCS and TBI?
The World Health Organization (WHO) defines health as the complete combination of mental, physical, and emotional health. The integral link between the three is the way our brain perceives and sends information throughout our body. As previously mentioned, our body has twice as many sensory neurons as motor neurons. They are used to signal our brain about what is happening in our environment, so it can send a chemical response, telling our body how to physically respond. When we are functioning at our optimum, these signals are accurate and delivered efficiently. However, when we experience a situation that we perceive as stressful (even unconsciously) our body may be signaled to transition into a “fight or flight” response even when no real threat exists. TBIs are complex conditions that manifest differently in each individual. However, based on personal experience, this response can frequently trigger throughout the day, leading to muscular contraction, rapid heart rate, anxiety, and compensation patterns.
Mindfulness, especially when cultivated through breath patterns, helps transition an individual’s automatic nervous system to neutral response, which is crucial for overall brain health. Thus, each session starts with mindfulness in order to calm the system so it can respond appropriately. The session then progresses into an individually tailored movement plan based on muscular imbalances and fascial restrictions that have resulted from unconscious compensations. Over time, we work together to restore physical functioning using a combination of yoga, Pilates, visualization, and advanced coordination.
How does mindful movement differ from craniosacral, neural, or visceral manipulation therapies?
Mindful movement is complementary to manipulation therapies. They are both used to support individual health through balancing someone’s system. Manual therapies offer individuals direct hands-on support, and even provide structural manipulation. Mindful movement, on the other hand, is a more hands-off approach. It builds strength and awareness by allowing an individual to sustain proper positioning while adapting to everyday movements. Most of the focus of sessions is building proper movement patterns, starting with core support.
A panacea does not exist, so it is my recommendation that individuals stay open to trying different approaches to see which ones work best for them. Don’t forget that you are allowed to pursue the ones you enjoy the most!
In the COVID era, are patients able to do virtual sessions effectively?
Overall, yes, but it is client-dependent. It was a seamless transition for clients who have established an in-person relationship. However, with an introductory session and a little trial and error, virtual sessions are opening the door to reaching people across the country. I am excited to be in the process of developing fully online and hybrid program options to help clients establish a strong mind-body connection within the comforts of their own home.
For those of you interested in contacting Kristi, please reach out to her on her website at mainsailwellness.com.
Kelly is a veteran, a writer, a TBI survivor, and a single mum of a girl child and a Frenchie, often found with oolong tea in one hand and humor in the other. She lives near Annapolis, Maryland.